Physical therapy SOAP note

Physical therapy SOAP notes are one part of thorough and accurate documentation of patient treatments.
Physical therapy SOAP notes are:
- A legal requirement of practicing physical therapy
- An important way to keep account of patient progress
- A method of communicating to co-treating therapists about a detailed plan of care
- A way to justify to payor sources that your treatments are medically necessary
- Defensible documents in case your notes become part of a legal case.
Physical therapy SOAP notes present a template for capturing (most) of the essential components of a daily visit and when used correctly, will give you the confidence to master your daily documentation. Sticking only to the components of physical therapy SOAP notes may result in incomplete documentation in some instances though. Read through to the end of this blog to find out when to elaborate a bit more.
What is a physical therapy SOAP note?
SOAP stands for subjective, objective, assessment and plan. In general, this formatting prompts the therapist to document the patient’s subjective report, the therapist’s objective findings and interventions, an assessment of the patient’s response to therapy and medical necessity for ongoing care, and the plan for subsequent visits. In this blog you will not only become more clear on the components of each section of the physical therapy SOAP note but also learn about other things you should always include to ensure your documentation is not incomplete.
Subjective (S)
This section of the physical therapy SOAP note should include the patient’s self-report of how they are feeling and their response to previous treatment(s). It may be appropriate to include subjective reports of caregivers or care partners here. Some self-report subjective outcome measures may be included in this section as well such as the SF-36 or the ABC.
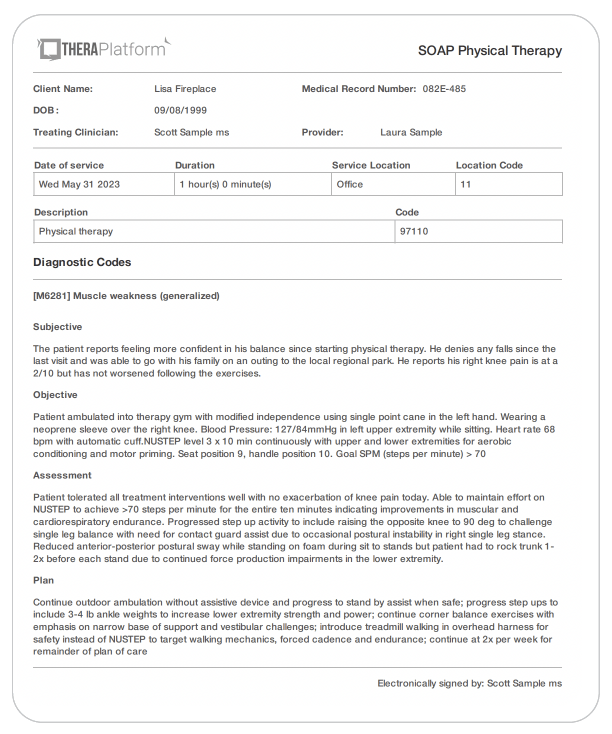
Subjective physical therapy SOAP note example: The patient reports feeling more confident in his balance since starting physical therapy. He denies any falls since the last visit and was able to go with his family on an outing to the local regional park. He reports his right knee pain is at a 2/10 but has not worsened following the exercises.
He also states that he saw his neurologist yesterday who cleared him to start driving. His recent brain MRI images show improving absorption of prior hemorrhage.
Objective (O)
The objective section of the physical therapy SOAP note consists of 3 distinct components.
- First, the therapist should document their objective findings made through observing the patient. For example, the therapist may list the patient’s blood pressure or heart rate, document an assistive device utilized by the patient or, describe the quality of movement observed in a particular joint.
- Second, this is the section where the therapist should list any objective tests and outcome measures administered to the patient and their results. Manual muscle testing, functional movement screens, and range of motion testing are examples of tests and measures the therapist may list here.
- Document your interventions here. Provide an account of the treatment provided and any pertinent information about patient response. Include the name of the intervention, number of sets and reps performed, intensity, equipment used (including how much or what type of resistance, if appropriate) and any modifications, cues or assistance provided to the patient. When documenting interventions it is good to think about writing in a way that would allow another therapist to step in and repeat your interventions without difficulty based only off of what you wrote in your note. Being too brief, using too many abbreviations or failing to document the equipment used would make it difficult for another therapist to recreate your treatment when creating this portion of the physical therapy SOAP note.
Objective physical therapy SOAP note example:
Observation: Patient ambulated into therapy gym with modified independence using single point cane in the left hand. Wearing a neoprene sleeve over the right knee.
Blood Pressure: 127/84mmHg in left upper extremity while sitting. Heart rate 68 bpm with automatic cuff
Objective testing
Timed up and go: 14.7s with single point cane and contact guard assist. ( <13s indicates reduced fall risk)
5x sit-to-stand test: 16.3s with no loss of balance, no UE push off (<12s indicates low fall risk)
Interventions
Therapeutic Exercise (28 min)
NUSTEP level 3 x 10 min continuously with upper and lower extremities for aerobic conditioning and motor priming. Seat position 9, handle position 10. Goal SPM (steps per minute) > 70
Donned gait belt
Step up to 6” box with LUE support on railing bringing trailing leg from floor to 90 degree hip flexion before stepping back down; 10 x 3 reps each side with contact guard assist, Rate of perceived exertion 5-6/10.
Sit to stand from 20” high mat table, feet on foam pad, holding 8# med ball with both hands with 5s pause once standing for balance challenge; 4x6 reps with stand by assist and 1 minute break between sets
NeuroMuscular Re-education direct with PT (30 min)
Corner balance exercises with PT stand by to contact guard assist with sturdy chair in front of patient: feet together with eyes open x 30s; feet together with eyes open + vertical and horizontal head turns x 10 each; feet together with eyes closed x 30s; feet together with eyes closed with vertical and horizontal head turns x 10 each; repeat 2 rounds of each activity without rest breaks
Single leg cone taps in standing; performed 10 taps in a row on right then left foot with verbal cues to increase contralateral weight shift; progressed to alternating cone taps 20x2 with contact guard to minimal assist
Over ground walking without assistive devices outdoors for 10 minutes over curbs, ramps, gravel, sidewalk and asphalt with 1x1 min standing rest break after five minutes. Contact guard assist at the gait belt and cues to look around for traffic when crossing the street.
Assessment (A)
The assessment section of a physical therapy SOAP note is where you demonstrate your skill in clinical decision making and problem solving. Simply stating that the patient “tolerated the treatment well” is not going to cut it. This section should include your professional thoughts on how the patient is responding to your interventions, possible precautions or barriers to rehab, remaining impairments and activity/participation restrictions and prognosis for responding to continued care.
Assessment physical therapy SOAP note example:
Patient tolerated all treatment interventions well with no exacerbation of knee pain today. Able to maintain effort on NUSTEP to achieve >70 steps per minute for the entire ten minutes indicating improvements in muscular and cardiorespiratory endurance. Progressed step up activity to include raising the opposite knee to 90 deg to challenge single leg balance with need for contact guard assist due to occasional postural instability in right single leg stance. Reduced anterior-posterior postural sway while standing on foam during sit to stands but patient had to rock trunk 1-2x before each stand due to continued force production impairments in the lower extremity.
Continues to show increased reliance on visual input with occasional loss of balance observed under eyes closed conditions and will benefit from continued exercises to improve utilization of vestibular input. Initiated outdoor walking without an assistive device today. Patient ambulates cautiously and needs cues to scan the environment more frequently to maintain safety around cars and other obstacles but did not demonstrate any losses of balance today though he should continue to use the device outside of therapy. He will benefit from continued skilled therapy to address impairments in strength, balance, endurance and motor control, reduce fall risk and increase independence and safety with mobility in the home and community.
Justifying the need for ongoing care is one of the most important components of this section. Patients, physicians and payor sources will be looking to this section to understand how the patient is benefiting from your interventions and why they are or are not making the expected progress. If the patient is not making the expected improvements on the tests and measures you list in the objective section but you fail to explain how extenuating circumstances or unforeseen barriers have impacted patient response you may find your patient’s care being cut short unexpectedly.
Assessment physical therapy SOAP note example: Today’s reassessment revealed that the patient has not made meaningful changes on the 6 Minute Walk Test and the 30s Chair Stand Test. While under normal circumstances this could suggest a poor response to physical therapy intervention, the patient is recovering from a bout of pneumonia for the last 2 weeks and is experiencing increased shortness of breath and fatigue as a result of the illness. He is expected to demonstrate more meaningful improvements at the next reassessment when he is back to his regular health and can perform at a higher level of intensity safely.
In another scenario, if you are confident your plan of care, patient education and interventions have been appropriate but your patient has not been doing their home exercise program and has been canceling appointments frequently despite (well-documented) conversations with the patient about how this will negatively impact their progress, the assessment section provides a place to explain why you may decide to discharge the patient before they have reached their goals without appearing as though you abandoned your patient needlessly. Your thorough documentation will show their performance on tests and measures across multiple sessions, their level of participation and your efforts as the therapist to educate them on the importance of adhering to the plan of care.
Start Your Free Trial Now
Plan (P)
The plan part of the physical therapy SOAP note should outline planned future services including interventions or patient education and if any changes to the original plan of care are expected.
Plan physical therapy SOAP note example:
Continue outdoor ambulation without assistive device and progress to stand by assist when safe; progress step ups to include 3-4 lb ankle weights to increase lower extremity strength and power; continue corner balance exercises with emphasis on narrow base of support and vestibular challenges; introduce treadmill walking in overhead harness for safety instead of NUSTEP to target walking mechanics, forced cadence and endurance; continue at 2x per week for remainder of plan of care.
Ensuring your documentation is complete
While the physical therapy SOAP note will help you to document most of your daily visit thoroughly, there are a few scenarios to keep in mind that should always be documented but don’t necessarily fit intuitively into the physical therapy SOAP note format.
- Collaboration or consultation with physicians, care partners, or other providers, for example, should always be documented in the patient’s chart.
- Additionally, reasons for cancellations and No Shows are important to document as it helps maintain a record of patient participation in therapy and external circumstances impacting their ability to adhere to your plan of care.
Failing to provide evidence of medical necessity and provision of skilled care are the top two reasons for denial of payment. To prove medical necessity, the therapist must document why therapy services are medically indicated at that exact time. Additionally, your notes must reflect why the services of a skilled therapist are necessary to deliver the intervention instead of another provider. How can you do this?
Start 30-day Free Trial and explore TheraPlatform. HIPAA Compliant Video and Practice Management Software for Therapists.
Here are a few tips:
- Document how specific interventions have resulted in progress toward your functional goals
- Document your clinical decision-making around why you prescribed, modified or discharged specific interventions
- Include in your assessment why your plan of care will address the body structure/function impairments and activity/participation restrictions that the patient is currently experiencing.
Mistakes to avoid during physical therapy SOAP note documentation
Now that you have a clearer understanding of the components to include in your physical therapy SOAP note, let’s consider some mistakes you want to avoid during documentation.
Taking care to avoid these mistakes will make your documentation more clear and concise when communicating why and how the patient is benefitting from your skilled therapy.
- Do not copy and paste the same information across multiple treatment sessions when using physical therapy SOAP notes; show that you are individualizing their care each time based off of your clinical assessment
- Save the assessment statements for the assessment section. Avoid adding assessment statements to the objective section as the objective section should be just the facts
- Make sure to attribute comments made by your patient or other family members in attendance to the person speaking when documenting in the subjective section of the physical therapy SOAP note. You want it to be clear who said what so it does not appear you are interjecting your opinion.
- Try to avoid restating information from the objective and subjective sections in the assessment as this can be repetitive but reference these items as needed to demonstrate your clinical reasoning for the plan of care.
While you may feel like the physical therapy SOAP note is more complicated than you realize, with a little practice implementing these guidelines you will become faster and more proficient. If you follow these suggestions, you can feel confident that your physical therapy SOAP note documentation will not only be thorough but will help facilitate consistent reimbursement of your services.
Simplifying physical therapy SOAP notes with an EMR tool
Creating efficient and secure physical therapy SOAP (Subjective, Objective, Assessment, and Plan) notes that are easy to store and share is a snap with TheraPlatform, an all-in-one EHR, practice management and teletherapy tool.
Easier physical therapy SOAP notes with templates and duplication
Using templates simplifies the physical therapy SOAP notes process and TheraPlatform provides a few ways to use their templates.
- Built-in template library: Browse TheraPlatform’s template library and choose the best note for your purposes. Therapists can easily utilize standardized SOAP note formats for efficient note-taking and ensure consistency and conciseness throughout documentation.
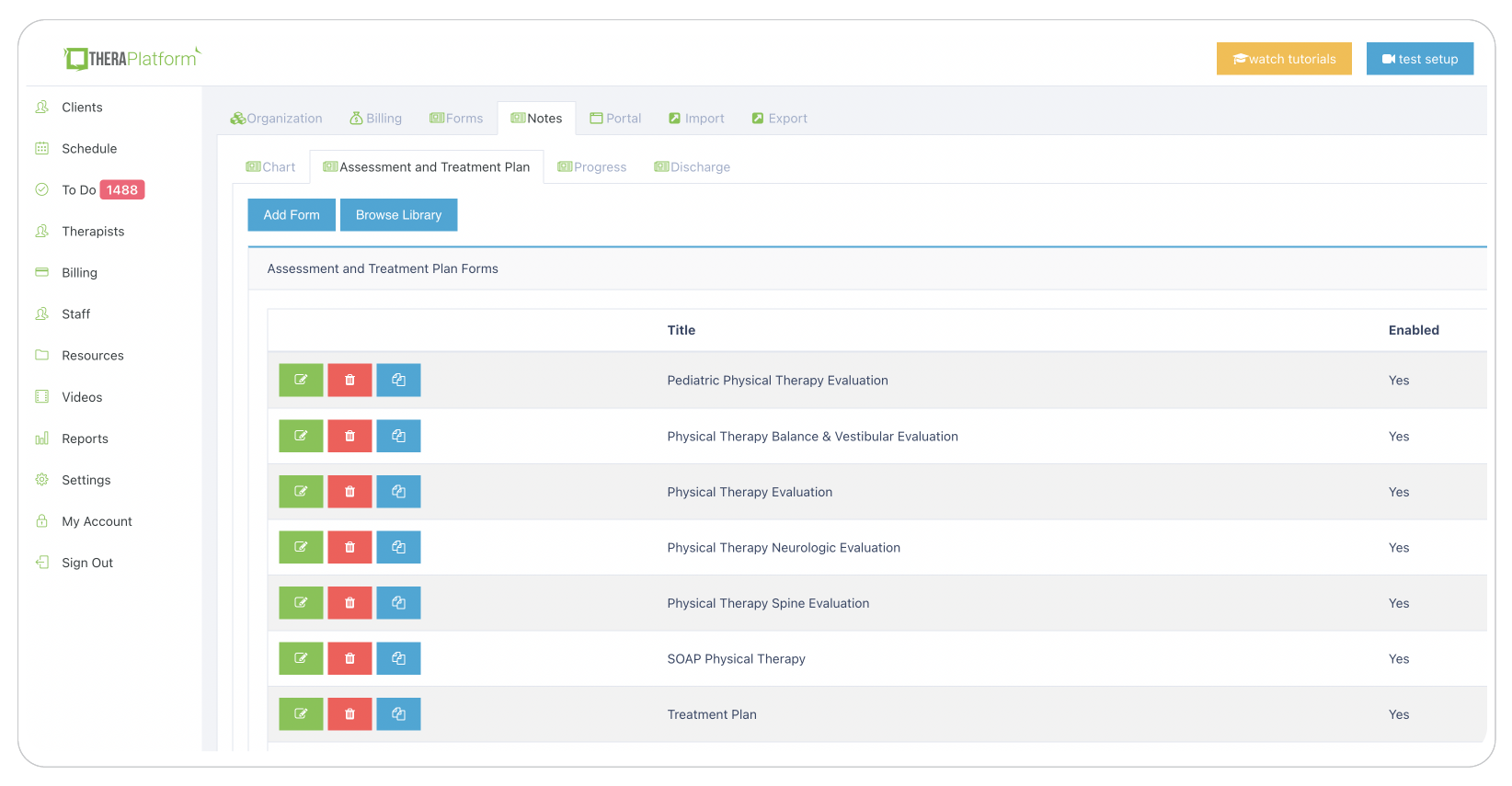
- Customizable note templates: TheraPlatform's flexible note template builder empowers physical therapists to customize SOAP note templates. Whether using traditional SOAP formats or personalized structures, PTs can tailor the templates to their specific needs.
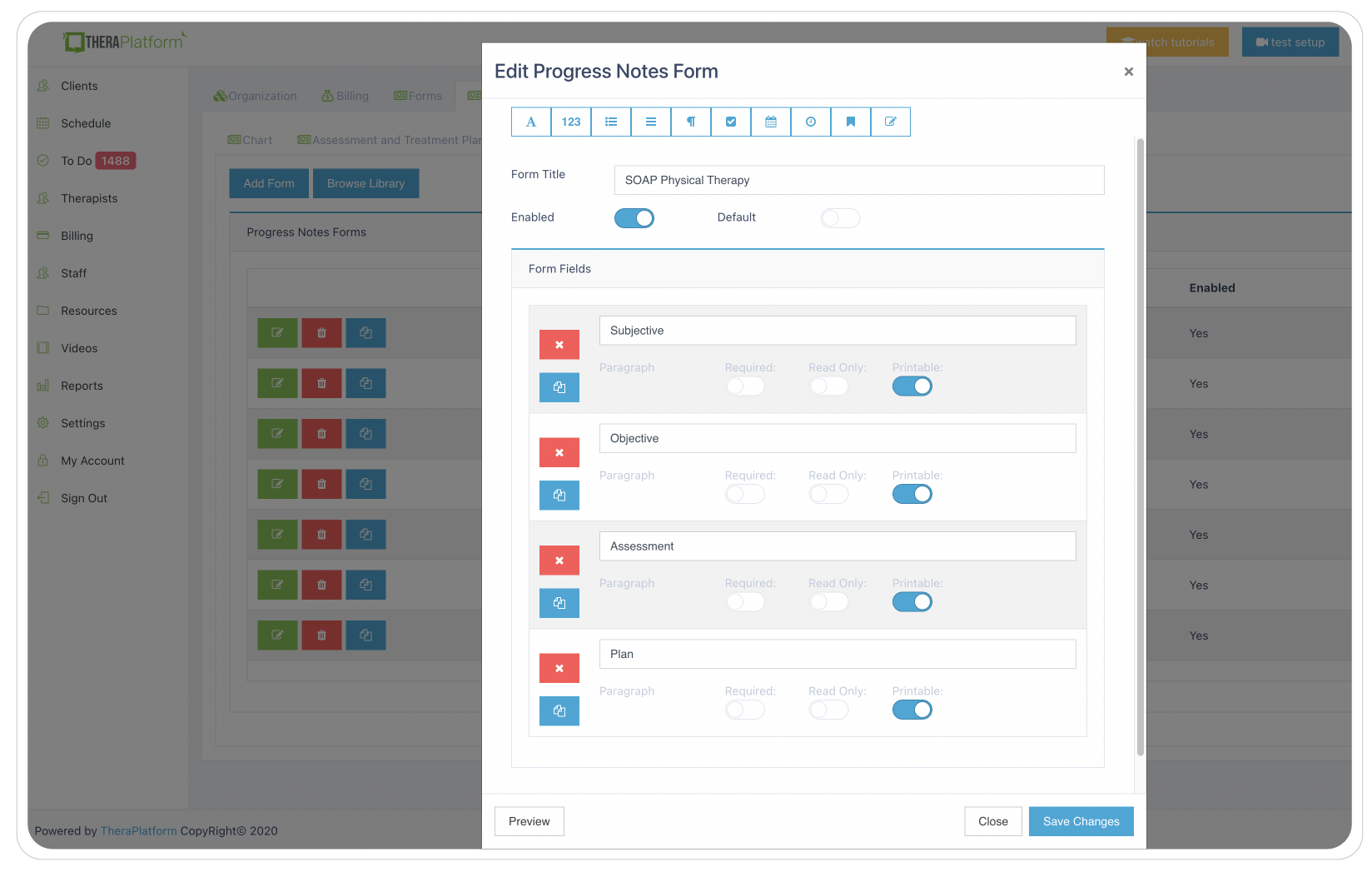
Duplication: Physical therapists can save time and maintain consistency by duplicating notes from previous sessions. This feature simplifies the documentation of recurring information or progress updates, allowing therapists to edit and expand upon the duplicated notes as necessary.
Accessing physical therapy SOAP notes
Easy access to organized physical therapy SOAP notes is a must for physical therapists as well as clients and other clinicians. TheraPlatform's easy-to-use EMR addresses the secure organization, storage, and accessibility of physical therapy SOAP notes through easy-to-use features.
Security
- HIPAA-Compliant and secure storage: TheraPlatform's EMR ensures secure storage by employing robust bank-level security measures to protect client data. Signed Business Associate Agreements (BAAs) further enhance the protection of Protected Health Information (PHI).
Accessibility
- Secure physical therapy SOAP notes sharing: TheraPlatform's EMR simplifies secure sharing of SOAP notes with clients through a HIPAA-compliant client portal. Clients can conveniently access their notes for personal records or insurance audits while maintaining confidentiality and privacy.
- Electronic signatures: TheraPlatform's Pro and Pro Plus plans enable therapists to request electronic signatures from providers or clients directly on physical therapy SOAP notes. Clients can easily download and print the signed documents, eliminating the need for physical signatures and paper-based processes.
- Integrated E-faxes: TheraPlatform's integration with efax services streamlines communication with clients and other providers by eliminating the need for separate platforms when sending or receiving SOAP notes. Therapists can seamlessly send and receive faxes directly from TheraPlatform, reducing administrative tasks and enhancing efficiency.
By utilizing TheraPlatform's EMR software for physical therapy SOAP note creation, security and accessibility therapists can save time, improve efficiency, and ensure HIPAA compliance. The software's template library, customizable note templates, duplication feature, secure storage, secure sharing through a client portal, electronic signatures, and integrated efax services contribute to a streamlined and effective SOAP notes process, ultimately enhancing the therapist's practice and client experience.
Resources
TheraPlatform, an all-in-one EHR, practice management and teletherapy tool, helps therapists streamline their physical therapy SOAP note documentation through pre-built templates and the ability to duplicate and customize notes across client care. They also offer a free, 30-day trial with no credit card required. Cancel anytime.
More resources
- How to start a physical therapy practice
- Common physical therapy ICD codes
- Therapy resources and worksheets
- Therapy private practice courses
- Ultimate teletherapy ebook
- The Ultimate Insurance Billing Guide for Therapists
- The Ultimate Guide to Starting a Private Therapy Practice