SIRP notes

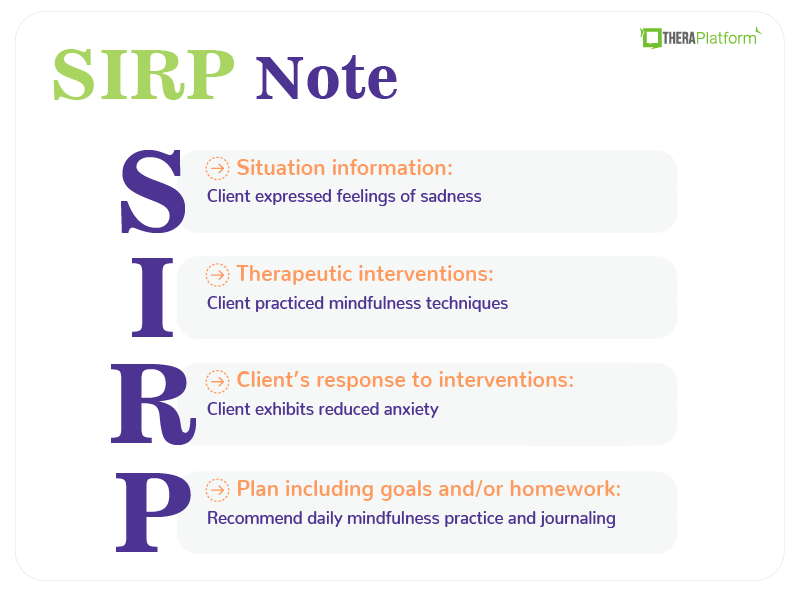
SIRP notes are a type of clinical documentation essential to mental health therapy. They provide a structured way to record client interactions, progress, and treatment plans. One of the widely used methods for clinical documentation is SIRP note, which stands for Situation, Interventions, Response, and Plan.
SIRP notes offer a concise and organized approach to documenting therapy sessions, ensuring that therapists can track their clients' progress and plan future interventions effectively.
Using SIRP notes ensures that documentation is systematic and thorough, covering all critical aspects of the therapy session. This method enhances clarity and consistency in clinical records, facilitating better communication between therapists, clients, and other healthcare providers. Additionally, SIRP notes help track therapy progress, identify patterns, and make informed decisions about treatment adjustments.
What is a SIRP Note?
Each section of the SIRP note serves a distinct purpose, contributing to a comprehensive and holistic view of the client's therapeutic journey.
SIRP is an acronym that stands for:
- Situation: Captures the client's subjective experiences, feelings, and perspectives as shared during the session and provides insight into the client's inner world.
- Interventions: Details the therapeutic interventions and techniques the therapist employs during the session.
- Response: This section records the client's response to the interventions, including any changes in behavior, mood, or insights gained, and captures the immediate effects of these strategies.
- Plan: Outlines the plan for future sessions, including goals, homework, and implementation strategies. It ensures continuity and focus in therapy.
These sections create a complete picture of the therapeutic process, facilitating better understanding, communication, and treatment planning.
Situation section of SIRP notes
Documenting the client's self-reported experiences, thoughts, and feelings
The Situation section of SIRP notes aims to capture the client's experiences, thoughts, and feelings during the therapy session. This involves noting the client's verbal accounts of their emotional state, mental processes, and any events or circumstances impacting their well-being.
For example, a client might share feelings of sadness, recount a stressful interaction at work, or describe their efforts to manage anxiety.
Capturing relevant information shared by the client
In this section, it's essential to document all pertinent information the client shares, including their current concerns and any updates on their progress since the last session. This can include changes in symptoms, new stressors, achievements, or setbacks.
Thorough documentation in the Situtation section ensures that the therapist comprehensively understands the client's current situation and can track changes over time.
Listening to reflect the client's situation accurately
Active listening and empathy are essential skills for accurately documenting the Situation section. By actively listening, therapists can ensure they fully understand the client's perspective, and by showing empathy, they can create a safe space for clients to express themselves openly. Reflecting on the client's experiences accurately in the notes helps build trust and ensures that the documentation represents the client's voice.
Interventions section of SIRP notes with example
The Interventions section details the therapist's therapeutic interventions and techniques during the session. These can include cognitive-behavioral strategies, mindfulness exercises, psychodynamic techniques, or any other methods applied. By clearly describing these interventions, therapists can record the approaches taken and assess their effectiveness over time.
Documenting the strategies used In this part of the note, the therapist should document how each intervention or technique addressed the client's concerns, goals, and treatment objectives. This could involve explaining the rationale behind choosing a particular intervention and how the therapist intended to help the client.
For instance, if the client is working on managing anxiety, the therapist might document the use of deep breathing exercises and cognitive restructuring to challenge anxious thoughts.
Tailoring interventions to match the client
One key aspect of effective therapy is tailoring interventions to fit each client's needs, preferences, and goals. In the Interventions section, it is important to note how the therapist customized strategies for the client.
This personalization ensures that the therapy is relevant and engaging for the client, increasing the likelihood of positive outcomes.
For example, if a client prefers mindfulness techniques over cognitive-behavioral ones, the therapist might prioritize mindfulness-based interventions in their sessions.
Response section of SIRP Notes
Evaluating the client's response to interventions and therapeutic techniques
The Response section evaluates how the client reacted to the interventions and therapeutic techniques used during the session. This involves observing and noting any immediate changes or reactions from the client. Did they appear more relaxed after a mindfulness exercise? Did they gain new insights from a cognitive-behavioral technique?
Evaluating these responses helps understand the interventions' impact on the client.
Documenting observed changes
In this section, it is important to document any changes in the client's symptoms, behaviors, or emotional state observed during the session. This can include improvements, deteriorations, or any other significant shifts.
For example, a client might exhibit reduced anxiety, increased engagement, or express a new understanding of their issues. These observations provide valuable data for assessing the client's progress and the effectiveness of the therapeutic approach.
Using objective measures and client feedback to assess effectiveness
Objective measures and client feedback are crucial for assessing the effectiveness of interventions. This can involve using standardized assessment tools, rating scales, or simply asking the client for feedback on how they felt about the interventions. By incorporating objective data and subjective feedback, therapists can understand how well the interventions work and make informed decisions about future sessions.
Watch this video to learn how to save time on therapy notes
→ Start My Free Trial
→ Start My Free Trial
Plan section of SIRP notes
Outlining the plan
The Plan section outlines the roadmap for future therapy sessions and sets ongoing treatment goals. This includes identifying the primary focus areas for the upcoming sessions and specifying the therapeutic goals. A clear plan gives the therapist and client a structured approach, ensuring that therapy remains goal-oriented and progressive.
Documenting action steps and recommendations
In this part of the note, the therapist documents specific action steps and recommendations for the client to implement between sessions. This can include homework assignments, coping strategies, or exercises to practice. These action steps reinforce the work done during sessions and promote continuous progress outside therapy.
For example, a therapist might recommend daily mindfulness practice or journaling thoughts and feelings.
Collaborating with the client
Collaboration with the client is key in developing a mutually agreed upon plan tailored to their needs and goals. This involves discussing and deciding on the next steps and ensuring the client is actively engaged in their treatment plan. By working together, the therapist and client can create a realistic, achievable plan aligned with the client's aspirations, enhancing motivation and commitment to the therapeutic process.
Synthesizing information from SIRP notes to develop a comprehensive case
SIRP notes provide a structured format that captures detailed information about the client's situation, interventions used, responses observed, and plans. By synthesizing this information, therapists can comprehensively understand the client's case. This involves analyzing patterns in the client's thoughts, emotions, and behaviors and integrating these insights to form a holistic view of the client's issues and progress.
Differentiating between SIRP notes and other clinical documentation formats
SIRP notes differ slightly from other clinical documentation formats, such as SOAP (Subjective, Objective, Assessment, Plan) notes or DAP (Data, Assessment, Plan), in a few ways.
While SOAP notes include an Objective section to record observable facts and an Assessment section for clinical impressions, SIRP notes focus more on the therapeutic process and client-centered documentation. The SIRP format emphasizes the client's subjective experience and the therapist's interventions and responses.
It is particularly well suited for mental health therapy where the client's perspective and the therapeutic relationship are central.
Theoretical perspectives and clinical observations in case conceptualization
Case conceptualization involves integrating theoretical perspectives and clinical observations to understand the client's presenting problems coherently. By combining insights from SIRP notes with relevant psychological theories and frameworks, therapists can identify underlying issues, formulate hypotheses about the client's difficulties, and understand the dynamics at play. This process helps in tailoring interventions that are theoretically sound and practically effective.
Using SIRP notes to guide treatment planning
SIRP notes are invaluable for guiding treatment planning and informing interventions in subsequent sessions. The detailed documentation of the client's responses to previous interventions and the outlined plans for future sessions provide a roadmap for ongoing therapy. Therapists can use this information to adjust their strategies, introduce new techniques, and set realistic and achievable goals for the client. This ensures that treatment is responsive to the client's evolving needs and promotes continuous progress.
SIRP notes examples
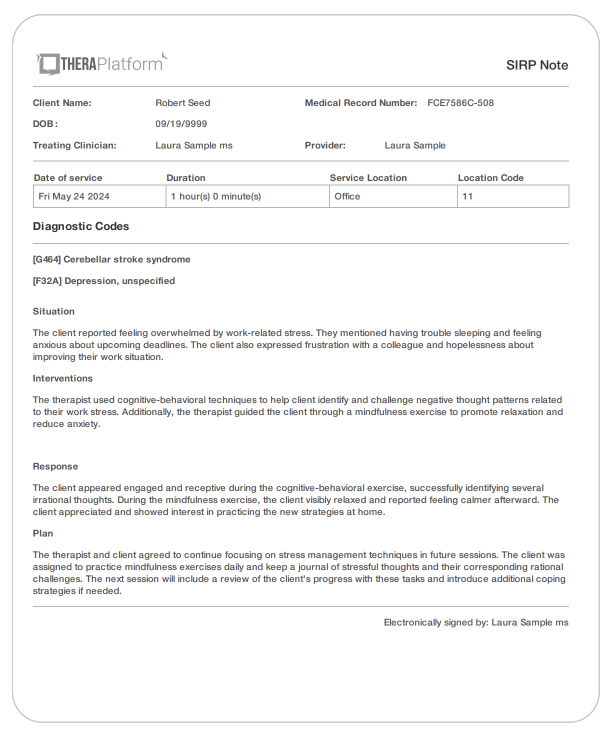
SIRP notes example note 1
Situation
The client reported feeling overwhelmed by work-related stress. They mentioned having trouble sleeping and feeling anxious about upcoming deadlines. The client also expressed frustration with a colleague and hopelessness about improving their work situation.
Interventions
The therapist used cognitive-behavioral techniques to help clients identify and challenge negative thought patterns related to their work stress. Additionally, the therapist guided the client through a mindfulness exercise to promote relaxation and reduce anxiety.
Response
The client appeared engaged and receptive during the cognitive-behavioral exercise, successfully identifying several irrational thoughts. During the mindfulness exercise, the client visibly relaxed and reported feeling calmer afterward. The client appreciated and showed interest in practicing the new strategies at home.
Plan
The counselor and client agreed to continue focusing on stress management techniques in future sessions. The client was assigned to practice mindfulness exercises daily and keep a journal of stressful thoughts and their corresponding rational challenges. The next session will include a review of the client's progress with these tasks and introduce additional coping strategies if needed.
SIRP notes example note 2
Situation
The client shared that they have been feeling more depressed over the past week, with low energy and a lack of interest in activities they usually enjoy. They also reported conflicts with their partner, which have been contributing to their low mood. The client mentioned feeling isolated and disconnected from their support network.
Interventions
The therapist used a person-centered approach to provide empathetic listening and validate the client's perspective. Additionally, the therapist introduced a behavioral activation strategy to help the client plan and engage in pleasurable activities to counteract their low mood.
Response
After the empathetic listening, the client appeared relieved and hopeful, expressing that they felt heard and understood. They showed interest in the behavioral activation strategy and collaborated with the therapist to create a list of activities they could try over the next week. The client reported feeling slightly more motivated to reconnect with their support network.
Plan
The therapist and client agreed to monitor the client's engagement in pleasurable activities and their impact on mood in the next session. The client was encouraged to contact at least one friend or family member during the week. The next session will review the client's experiences with these activities, address any barriers, and explore further strategies for improving mood and relationship dynamics.
→ Download My Free SIRP Notes Template
Documentation best practices
Accurate, clear, and professional documentation is crucial in maintaining the integrity and utility of SIRP notes. Therapists should ensure that each note precisely reflects the session's content, avoiding vague language and ambiguous statements. Professionalism in writing, including proper grammar and respectful language, is essential to upholding the standards of clinical practice.
Adhering to legal and ethical guidelines
Therapists must adhere to legal and ethical guidelines to protect client confidentiality and privacy when documenting SIRP notes. This includes ensuring that records are securely stored and only accessible to authorized individuals. Therapists should avoid including unnecessary details that could compromise the client's privacy and always obtain informed consent before sharing any information.
Incorporating client feedback and self-report data
Incorporating client feedback and self-report data enhances the accuracy and relevance of SIRP notes. Therapists should actively seek and document the client's perspectives on their progress, experiences, and the effectiveness of interventions. This collaborative approach ensures that the notes reflect the client's voice and provide valuable insights for ongoing treatment planning.
Training and implementation
Proper education and training are beneficial for therapists to use SIRP notes effectively. Training programs should cover the purpose and structure of SIRP notes, best practices for documentation, and common pitfalls to avoid. Hands-on training with real-life examples can help therapists understand how to apply the SIRP format.
Offering supervision and support
Ongoing supervision and support are critical for therapists to develop proficiency in SIRP note documentation. Regular feedback from mutually agreed-upon plans and skills addresses challenges and improves the quality of their notes. Peer support and discussion groups can also provide valuable opportunities for learning and sharing best practices.
Encouraging ongoing reflection and a realistic, achievable plan
Therapists are encouraged to continuously engage in ongoing reflection and self-assessment to improve their documentation skills. This can involve reviewing their notes, seeking feedback from colleagues, and staying updated on current best practices and guidelines in clinical documentation. Self-assessment tools and reflective exercises can support therapists in identifying areas for improvement and enhancing their competency in using SIRP notes.
Ethical and legal considerations
Addressing ethical dilemmas and challenges in SIRP note documentation
Documenting SIRP notes can raise ethical dilemmas and challenges. Therapists must navigate these issues carefully, ensuring their documentation practices uphold ethical standards and prioritize the client's best interests. This can involve seeking supervision or consultation when faced with complex ethical decisions and adhering to professional guidelines.
Maintaining confidentiality and privacy
Maintaining confidentiality and privacy is paramount in documenting sensitive client information. Therapists should use de-identified information where appropriate and record sensitive details with discretion. Secure storage systems and strict access controls are essential to protect client records from unauthorized access.
Regulatory requirements and professional standards
Therapists must adhere to regulatory requirements and professional standards in their clinical documentation. This includes understanding and complying with relevant laws and regulations, such as HIPAA in the United States, and following guidelines set forth by professional organizations such as the APA. Regular training and updates on legal and regulatory changes can help therapists stay compliant and ensure that their documentation practices are up-to-date.
SIRP notes, with their structured format of Subjective, Interventions, Response, and Plan, provide an effective method for clinical documentation in mental health therapy. Each section captures crucial aspects of the therapeutic process, ensuring a comprehensive record of client sessions.
The systematic approach of SIRP notes enhances clarity, consistency, and thoroughness in documentation. This structured method supports better treatment planning, facilitates tracking of client progress, and improves communication between therapists and other healthcare providers, ultimately enhancing client care and treatment outcomes.
Mental health therapists are encouraged to adopt and implement SIRP notes in their clinical practice. By doing so, they can ensure high-quality documentation that supports effective therapy, meets ethical and legal standards and contributes to positive client outcomes.
Start 30-day Free Trial and explore TheraPlatform. HIPAA Compliant Video and Practice Management Software for Therapists.
How EMR software can help with psychotherapy notes
Electronic medical record (EMR) and practice management software, such as TheraPlatform, can make note-taking fast, flexible, and accurate.
Benefits of using EMR for psychotherapy notes
Consistent notes with a library of note templates
Having an EMR with built-in note templates, such as SIRP, SOAP, BIRP, or DAP, can help psychotherapists write more consistent and concise therapy notes and stay organized.
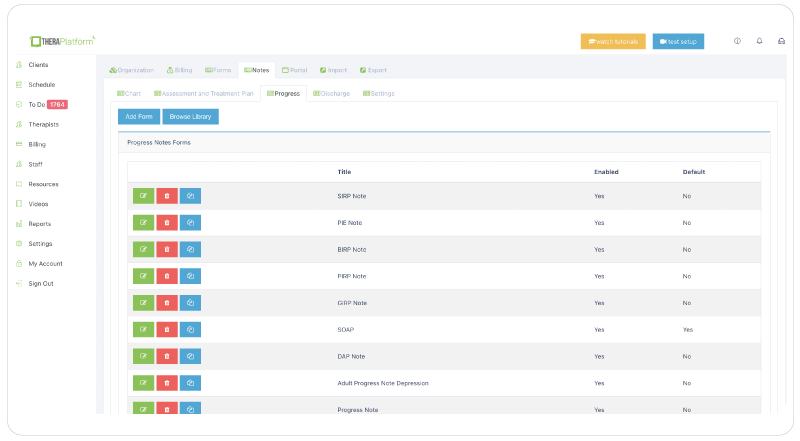
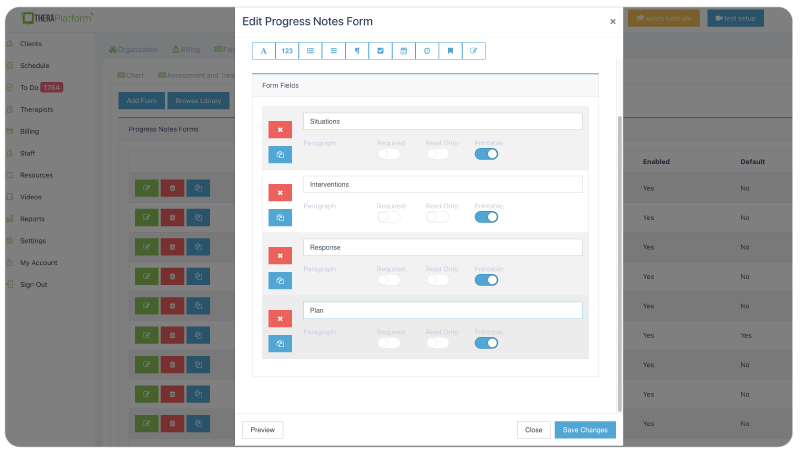
Flexible note template builder
Psychotherapists have their way of documenting sessions. Some love SIRP note templates to help organize Subjective, Intervention, Response, and Plan. Other psychotherapists prefer a single field that allows them to craft their narrative. Other psychotherapists use checkboxes on their note templates for repetitive information such as techniques or mental status. Using a comprehensive, easy-to-use note template builder is the key to flexibility.
HIPAA-compliant storage of psychotherapy notes
Creating and storing psychotherapy notes in a secure, encrypted system to prevent breaches will ensure your client's data is safe and give you peace of mind. TheraPlatform follows bank-level security standards and provides private practices with a signed BAA.
Securely and easily share your psychotherapy notes with clients
Clients on your caseload may request psychotherapy notes for their own records, and superbill clients may need them in case of an insurance audit. Having a secure way to share your notes is an easy decision.
Mental health therapy SOAP notes are created with TheraPlatform. Therapists can share notes with clients with a few clicks of a button.
Electronically request signatures from your clients on your psychotherapy notes
TheraPlatform's Pro and Pro Plus plans offer documentation features, including the ability to request client signatures on notes. Your client can also download and print this document.
Duplicate notes from previous sessions
Some information that psychotherapists include in SOAP notes might repeat from session to session, and a copy note feature on TheraPlatform allows clinicians to duplicate notes from previous sessions. Therapists can edit the copied note to add or delete information.
Pre-populated treatment plans
Through Wiley Treatment Planner integration, creating treatment plans in TheraPlatform is also a great time saver. Psychotherapists can customize treatment plans with over 1,000 clear statements describing behavior. They can also access reliable, evidence-based objectives and interventions and receive home suggestions to assign to clients.
Fax your notes from your clients' chart with a click of a button
Eliminate maneuvering between two services with an integrated solution, such as TheraPlatform, which has fax integrated into its EMR. This integration saves time and lowers costs, as incoming and outgoing documents, such as SOAP notes and other documents, are sent via fax.
Resources
Theraplatform is an all-in-one EHR, practice management and teletherapy solution that allows you to focus more on patient care. With a 30-day free trial, you have the opportunity to experience Theraplatform for yourself with no credit card required. Cancel anytime. They also support different industries including mental and behavioral health therapists in group practices and solo practices.

More resources
- Therapy resources and worksheets
- Therapy private practice courses
- Ultimate teletherapy ebook
- The Ultimate Insurance Billing Guide for Therapists
- The Ultimate Guide to Starting a Private Therapy Practice
- Mental health credentialing
- Insurance billing 101
- Practice management tools
- Behavioral Health tools
Free video classes
- Free on-demand insurance billing for therapist course
- Free mini video lessons to enhance your private practice
- 9 Admin tasks to automate in your private practice
References
Luepker, E. T. (2012). Documenting psychotherapy: Essentials for mental health practitioners (2nd ed.). Routledge.
Glick, R. L., Berlin, J. S., & Morse, S. J. (2011). Clinical documentation in behavioral health. PESI Publishing & Media.
Wiger, D. E. (2011). The essentials of clinical documentation. Wiley.



